As the country moves through the summer, countless families, parents, and educators are scrambling to figure out how to appropriately communicate to their children about what is going on in a way that they will comprehend, but not overwhelm. This has proved challenging as these are unprecedented times, where even as adults, we don’t necessarily know what lies ahead. Parents and educators are trying their best to organize school related summer activities, prepare for the next school year, and communicate to the children what their school year could look like going forward. This can be overwhelming for adults and children, especially if you do not have proper guidance, information, and resources to communicate effectively.
Below you will find resources pertaining to adults and children, and what they can do to better understand and prevent the spread of COVID-19.
Smithsonian
“COVID-19! How Can I Protect Myself and Others? will help you, and your community, understand the science of the virus that causes COVID-19 and other viruses like it. It will help you to figure out how this virus is impacting or affecting you or may impact you in the future. It will help you to understand the actions that you can take to keep yourself and your community safe.
In this project, you will discuss how people feel about the virus. You will investigate the science of this virus. You will explore public health measures, which are things that are happening in your community or may happen soon to keep COVID-19 from spreading. You will take action to support health in your community.
Help us measure impact! By providing us with this basic information, you are ensuring that we can document the reach of the COVID-19 module, and help the Smithsonian Science Education Center to understand how to best support educators and parents as they undertake this module with their learners” Click here
My Hero is You, Storybook for Children on COVID-19
“This book was a project developed by the Inter-Agency Standing Committee Reference Group on Mental Health and Psychosocial Support in Emergency Settings (IASC MHPSS RG). The project was supported by global, regional and country based experts from Member Agencies of the IASC MHPSS RG, in addition to parents, caregivers, teachers and children in 104 countries. A global survey was distributed in Arabic, English, Italian, French and Spanish to assess children’s mental health and psychosocial needs during the COVID-19 outbreak. A framework of topics to be addressed through the story was developed using the survey results. The book was shared through storytelling to children in several countries affected by COVID-19. Feedback from children, parents and caregivers was then used to review and update the story.
Over 1,700 children, parents, caregivers and teachers from around the world took the time to share with us how they were coping with the COVID-19 pandemic. A big thank you to these children, their parents, caregivers and teachers for completing our surveys and influencing this story. This is a story developed for and by children around the world”
For access to the storybook go to the link below (multiple language versions are available and downloadable)
Centers for Disease Control and Prevention-Talking with children about Coronavirus Disease 2019
Tips for talking with children (CDC)
Remain calm. Remember that children will react to both what you say and how you say it. They will pick up cues from the conversations you have with them and with others.
Reassure children that they are safe. Let them know it is okay if they feel upset. Share with them how you deal with your own stress so that they can learn how to cope from you.
Make yourself available to listen and to talk. Let children know they can come to you when they have questions.
Avoid language that might blame others and lead to stigma.
Pay attention to what children see or hear on television, radio, or online. Consider reducing the amount of screen time focused on COVID-19. Too much information on one topic can lead to anxiety.
Provide information that is truthful and appropriate for the age and developmental level of the child. Talk to children about how some stories on COVID-19 on the Internet and social media may be based on rumors and inaccurate information. Children may misinterpret what they hear and can be frightened about something they do not understand.
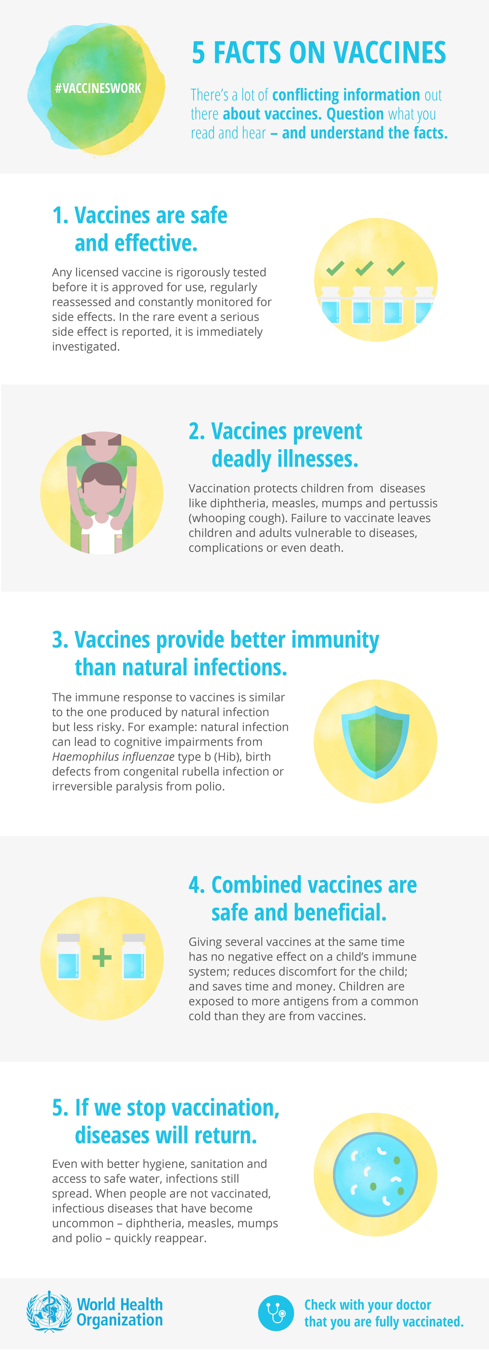
Teach children everyday actions to reduce the spread of germs. Remind children to wash their hands frequently and stay away from people who are coughing or sneezing or sick. Also, remind them to cough or sneeze into a tissue or their elbow, then throw the tissue into the trash.
If school is open, discuss any new actions that may be taken at school to help protect children and school staff.
Messages for parents, school staff, and others working with children
Centers for Disease Control and Prevention Caring for Children during COVID-19
Based on available evidence, children do not appear to be at higher risk for COVID-19 than adults. While some children and infants have been sick with COVID-19, adults make up most of the known cases to date.
Watch your child for any signs of COVID-19 illness
COVID-19 can look different in different people. For many people, being sick with COVID-19 would be a little bit like having the flu. People can get a fever, cough, or have a hard time taking deep breaths. Most people who have gotten COVID-19 have not gotten very sick. Only a small group of people who get it have had more serious problems.
CDC and partners are investigating cases of multisystem inflammatory syndrome in children (MIS-C) associated with COVID-19. Learn more about COVID-19 and multisystem inflammatory syndrome in children (MIS-C).
Keep children healthy (CDC)
Teach and reinforce everyday preventive actions
Parents and caretakers play an important role in teaching children to wash their hands. Explain that hand washing can keep them healthy and stop the virus from spreading to others.
Be a good role model—if you wash your hands often, they’re more likely to do the same.
Learn more about what you can do to protect children.
Help your child stay active
Encourage your child to play outdoors—it’s great for physical and mental health. Take a walk with your child or go on a bike ride.
Use indoor activity breaks (like stretch breaks or dance breaks) throughout the day to help your child stay healthy and focused.
Help your child stay socially connected
Reach out to friends and family via phone or video chats.
Write cards or letters to family members they may not be able to visit.
Some schools and non-profits, such as the Collaborative for Academic, Social, and Emotional Learningexternal icon and The Yale Center for Emotional Intelligenceexternal icon, have resources for social and emotional learning. Check to see if your school has tips and guidelines to help support social and emotional needs of your child.
Ask about school meal services
Check with your school on plans to continue meal services during the school dismissal. Many schools are keeping school facilities open to allow families to pick up meals or are providing grab-and-go meals at a central location.
Help your child cope with stress
Watch for signs of stress or behavior changes
Not all children and teens respond to stress in the same way. Some common changes to watch for include:
Excessive worry or sadness
Unhealthy eating habits
Unhealthy sleeping habits
Difficulty with attention and concentration
Support your child
Parents can find more information about supporting their children during a COVID-19 outbreak on CDC’s Helping Children Cope page.
Talk with your child or teen about the COVID-19 outbreak. Answer questions and share facts about COVID-19 in a way that your child or teen can understand.
Learn more about common reactions that children may have and how you can help children cope with emergencies.